Which Type of Dental Implant has the Highest Success Rate?
If you're reading this, you may be considering dental implants, and wondering which type has the highest success rate. The loss of one or more teeth can negatively impact your ability to eat and speak naturally. Fortunately, good dental implants offer a permanent and practical solution for restoring oral function and aesthetics for people with missing teeth. These artificial tooth roots are surgically implanted in the jaw to support dental prosthetics, such as crowns and bridges. The success rate of dental implants is quite high but selecting the right dental implant is a must for a successful outcome. Understanding the success rate of different types of implants can help you make an informed decision about your treatment.
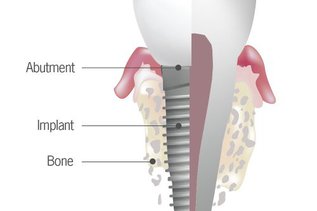
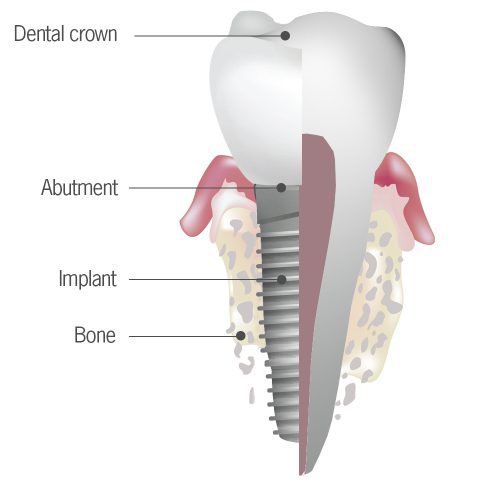
What Are Dental Implants?
Dental implants are screw-like posts made with biocompatible materials, like titanium or zirconia. Once implanted in the jaw, they fuse with the surrounding bone through the process of osseointegration. This creates a stable foundation for a replacement or prosthetic tooth. Dental implants present numerous advantages over conventional tooth replacement choices. Some of these benefits include better function, bone structure preservation, and a more natural appearance.
Key Benefits of Dental Implants
- Natural Look and Feel: Implants closely mimic the appearance and function of real teeth.
- Preserve Jawbone Structure: They prevent bone loss that commonly occurs after tooth loss.
- Improved Functionality: Implants restore full chewing ability, unlike removable dentures.
- Long-Term Durability: With proper care, dental implants can last for decades.
- Boosted Confidence: They offer a secure, aesthetic solution that improves speech and self-esteem.
Types of Dental Implants
Several types of dental implants are available today, each designed to suit different clinical needs, bone conditions, and aesthetic goals. Your dentist will recommend the best option based on your individual situation.
Endosteal Implants (Most Common)
Endosteal implants are the most widely used type of implant. These screw-shaped posts are surgically placed into the jawbone. Over time, they integrate with the surrounding bone tissue through a process known as osseointegration, providing a solid anchor for crowns, bridges, or dentures. This type is ideal for patients with good bone density and overall oral health.
Subperiosteal Implants
Subperiosteal implants are positioned on top of the jawbone but beneath the gum tissue. They are often used when patients lack sufficient bone height or volume and are not suitable candidates for bone grafting. This type consists of a custom metal framework that holds the prosthetic teeth in place.
Single-Tooth Implants
A single-tooth implant is used to replace one missing tooth. A titanium or zirconia post is inserted into the jawbone, and a crown is placed on top. This solution preserves adjacent teeth, offering a natural look and function without compromising the surrounding structures.
Multiple-Tooth Implants
When two or more teeth are missing, multiple-tooth implants can support a fixed bridge or a partial denture. This method involves placing two or more implants, which serve as anchors for several prosthetic teeth. It offers a stable, long-lasting alternative to removable dentures.
Full-Arch Implants (All-on-4 or All-on-6)
Full-arch implants are designed for patients who have lost most or all of their teeth. This method involves placing four to six strategically positioned implants in each jaw to support an entire arch of prosthetic teeth. Known as the All-on-4 or All-on-6 system, it provides a full set of fixed teeth that look and feel natural. It is a reliable and time-efficient solution for full-mouth rehabilitation.

Success Rates by Implant Type
So, what is the success rate of dental implants? Numerous studies have been conducted to assess the success rates of different types of dental implants. While success rates can vary depending on individual circumstances as described above, some general trends can be seen.
Endosteal Implants (Standard Screws)
✅ Success Rate: Approximately 90–95% over 10 years
Endosteal implants are the most commonly used and are considered the gold standard in dental implantology. Their high success rate is attributed to their integration with the jawbone through osseointegration. With proper oral hygiene and regular dental visits, they can last a lifetime.
Subperiosteal Implants
✅ Success Rate: Approximately 80–90% over 5 years
Subperiosteal implants are placed on top of the jawbone and are typically used in patients with insufficient bone height who cannot undergo bone augmentation procedures. While less common today, they remain a viable option for some instances. Their success depends heavily on proper fit, hygiene, and the absence of chronic health issues.
Single-Tooth Implants
✅ Success Rate: Approximately 95–97% over 10–15 years
Single-tooth implants are ideal for replacing a single missing tooth and offer highly predictable outcomes, especially when placed early after tooth loss. Long-term maintenance is minimal with proper brushing and flossing.
Multiple-Tooth Implants (Bridges or Dentures)
✅ Success Rate: Typically above 90% over 10 years
Multiple-tooth restorations using implants show consistently strong outcomes. However, the success may vary based on the number of implants placed, bone condition, and whether the prosthetic is fixed or removable. Proper planning and execution are crucial for optimal results.
Full-Arch Implants (All-on-4 or All-on-6)
✅ Success Rate: Approximately 94–98% over 10+ years
Full-arch restorations, such as All-on-4, are highly effective for patients who have lost most or all of their teeth. With just 4–6 implants per jaw, they provide immediate function and long-lasting aesthetics. Proper hygiene and professional care are key to their longevity.
Factors That Affect Implant Success
Dental implant success isn't guaranteed solely by the procedure. Several key factors influence the integration of an implant with the jawbone and its longevity. Understanding these elements can help patients and dentists plan for better outcomes.
Jawbone Density and Quality
The density and volume of the jawbone are among the most critical determinants of implant success. A healthy, thick jawbone provides better support for osseointegration — the process by which the implant fuses with the bone. Patients with low bone density may require bone grafting before implant placement to increase the likelihood of success.
Implant Size and Length
The dimensions of the implant play a vital role in its stability and strength. Longer and wider implants typically provide a greater surface area for bone contact, thereby enhancing integration and load-bearing capacity. However, available bone structure and anatomical limits must be considered when selecting the right size.
Age and Health of the Patient
While there’s no upper age limit for dental implants, overall health is more important than age. Conditions like uncontrolled diabetes, autoimmune disorders, or poor oral hygiene can compromise healing. Smoking also significantly reduces the success rates of implants. A thorough medical history and lifestyle evaluation are essential before surgery.
Placement Location (Front vs Back Teeth)
Implants placed in the back of the mouth (molars) are subject to stronger chewing forces than those in the front. As a result, the implant site affects both design and success probability. Denser bone in the anterior (front) regions often supports quicker healing, while posterior implants may require additional planning and support.
Dentist’s Experience and Technique
The skill and experience of the dental surgeon have a direct impact on the success of implants. A trained professional with expertise in implantology will assess anatomical nuances, use advanced imaging for precise placement, and ensure sterile technique. Choosing a qualified dentist significantly reduces the risk of complications and enhances long-term outcomes.
Implant Materials and Their Role
The dental implant material can also affect its success. Excellent biocompatibility and strength make titanium and its alloys make for the most commonly used and successful materials. Patients with allergies or aesthetic concerns may be recommended Zirconia implants.
Titanium alloy implants typically show slightly higher success rates, compared to zirconia implants. This is especially true in cases with poor bone quality or complex anatomical conditions.
Advances in Dental Implant Technology
Modern innovations have transformed the planning, placement, and integration of dental implants, resulting in higher success rates and shorter recovery times. Below are the key technological advancements driving this progress:
Digital Planning and 3D Imaging
Advanced diagnostic tools like cone-beam computed tomography (CBCT) and 3D intraoral scanners allow dentists to plan implant placement with remarkable precision. These technologies provide detailed images of the patient’s bone structure, nerves, and sinuses, enabling safer, more accurate procedures. Computer-guided surgery based on these scans minimizes surgical trauma and reduces the margin of error.
Immediate Loading Protocols
Traditionally, implants required several months to integrate before they could support a prosthetic tooth. Now, with immediate loading protocols, a temporary crown can often be placed on the same day as the implant surgery. This reduces overall treatment time and provides immediate aesthetic and functional benefits. However, it requires excellent bone quality and careful case selection to ensure a successful outcome.
Surface Enhancements (e.g., SLA, SLActive)
Recent surface treatment technologies have significantly enhanced the bonding of implants with bone. Techniques such as sandblasting, large grit, Acid Etching (SLA), and its hydrophilic variant, SLActive, enhance the implant’s surface area and promote faster osseointegration. These treated surfaces attract bone-forming cells and improve early healing outcomes, particularly in patients with compromised bone quality.

Who Is a Good Candidate for Dental Implants?
Dental implants are an excellent solution for many people; however, not everyone is an ideal candidate immediately. Successful implant placement depends on several factors, including overall health, jawbone quality, and oral hygiene. Understanding who makes a good candidate can help you prepare for the procedure and improve the chances of a long-lasting, successful outcome.
Checklist for Ideal Candidates
- Good general health: Candidates should be free from uncontrolled chronic illnesses such as diabetes or immune disorders that could impair healing.
- Sufficient jawbone density and volume: Adequate bone is crucial to anchor the implant securely.
- Healthy gums: Healthy gum tissue free from periodontal disease supports implant success.
- Non-smoker or willing to quit: Smoking can significantly increase the risk of implant failure by impairing blood flow and healing.
- Commitment to oral hygiene: Maintaining good oral hygiene and regular dental visits is essential for long-term implant health.
- Realistic expectations: Candidates should understand the process, timeline, and maintenance involved with implants.
When Additional Procedures May Be Needed (Bone Graft, Sinus Lift)
Some patients may require preparatory procedures if they lack sufficient bone or have other anatomical limitations.
- Bone grafting: This procedure rebuilds or augments the jawbone to provide a stable base for implants. It uses bone from the patient, a donor, or synthetic materials.
- Sinus lift: For upper jaw implants near the sinus cavities, a sinus lift may be necessary to elevate the sinus floor and create sufficient bone height for implant placement.
Both procedures add time to the treatment plan but significantly improve the chances of implant success in patients with insufficient bone.
Choosing the Right Implant
There is no solution that is good for everyone when it comes to choosing the best dental implants. The implant process begins with a complete evaluation of the patient's specific needs, bone quality, medical history, and preferences.
The experienced dental implant team at North York Smile Center employs a custom approach to treatment planning, ensuring that each patient receives the most suitable implant and best treatment for their unique needs. Your dentist will do the following:
- Complete oral health examination to assess your overall oral health, bone density, and your overall health to determine the best implant for you
- Customized treatment for your unique needs and goals
- Address your concerns so you can feel comfortable throughout the process
Dental implants can restore the function, and appearance, that people with missing teeth long for.
Frequently Asked Questions
How long do dental implants last?
With proper care, dental implants can last 20 years or more. Success depends on maintaining good oral hygiene, attending regular dental check-ups, and avoiding habits such as smoking.
Is the dental implant procedure painful?
Most patients experience minimal discomfort during and after the procedure. Local anesthesia and sedation options help ensure a comfortable experience.
How long does it take to get dental implants?
The entire process can take several months, including healing time. Some cases utilize immediate loading, which allows for a temporary tooth to be placed on the same day.
Can dental implants fail? What are the risks?
While dental implants have a high success rate, risks include infection, implant rejection, or failure to integrate with the bone. Choosing an experienced dentist minimizes risks.
What is the difference between endosteal and subperiosteal implants?
Endosteal implants are placed directly into the jawbone and are the most common. Subperiosteal implants rest on top of the jawbone and are used when bone density is insufficient.
Will I need a bone graft before getting implants?
Some patients require bone grafting or sinus lifts if they lack enough bone for stable implant placement. Your dentist will evaluate and recommend these procedures if necessary.
Does insurance cover dental implants?
Some dental insurance plans offer partial coverage for implants, but many do not. It’s best to check your specific plan and discuss financing options with your dental office.
Resources:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6212375/#:~:text=At%201%2Dyear%20follow%2Dup,and%20platform%2Dmatching%20implants%20respectively.
- https://www.ncbi.nlm.nih.gov/books/NBK470448/
- https://www.researchgate.net/publication/262680887_Current_trends_in_dental_implants
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979349/
- https://onlinelibrary.wiley.com/doi/10.1111/j.1600-0501.2012.02546.x
- https://pubmed.ncbi.nlm.nih.gov/24660189/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8199359/

